Everyone has heard the cautions regarding the use of opioids such as fentanyl, oxycodone, and morphine. Millions of people who suffer from chronic ailments, injuries, or surgeries can find respite from them as potent painkillers.
But behind their promise of comfort lies a disturbing reality: opioids carry serious risks that aren’t always apparent until it’s too late.
While many patients experience only temporary nausea or drowsiness, for some, the consequences of opioid use can spiral into a nightmare with lifelong impacts.
As doctors prescribe ever larger doses for longer periods, more patients are discovering that what started as medication can all too easily become something far more menacing. It’s time to shine a light on the troubling side effects opioids may unleash when used as a long-term treatment for pain.
What Are Opioids?
The projected growth of the Global Opioids Market indicates a significant increase in value, estimated to reach approximately USD 29.5 Billion by 2033, up from USD 22.2 Billion in 2023. This growth is forecasted to occur at a Compound Annual Growth Rate (CAGR) of 2.9% between 2024 and 2033.
But what are they anyway?
Opioid medications, also known as narcotic analgesics, play a crucial role in managing severe or persistent pain as prescribed by healthcare professionals. These medications are commonly recommended for patients suffering from various conditions such as chronic headaches, back pain, cancer-related discomfort, or injuries resulting from accidents or sports activities.
When administered under medical supervision and in appropriate doses, opioid pain relievers have demonstrated effectiveness in alleviating pain symptoms.
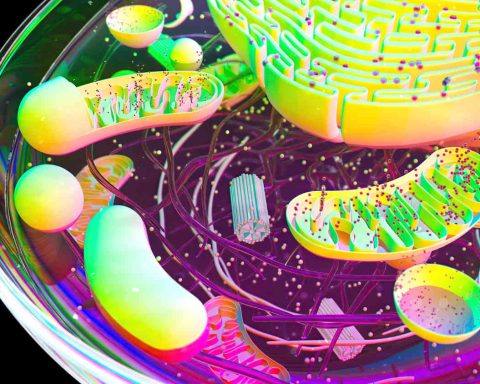
The mechanism of action of opioid medications involves binding to protein receptors located on nerve cells in key areas of the body, including the brain, spinal cord, and gut. Through this interaction, opioid drugs activate the receptors, effectively blocking the transmission of pain signals from injury or inflammation sites to the brain via the spinal cord pathway.
While offering significant pain relief benefits, it’s important to acknowledge the associated risks, such as potential misuse, abuse, and addiction, particularly when these medications are used for prolonged periods in chronic pain management scenarios.
To mitigate these risks, close monitoring and supervision by healthcare providers are essential when opioid therapy is deemed medically necessary.
What Are the Types of Opioids?
Opioid medications represent a group of drugs that include illegal narcotics like heroin as well as both natural and synthetic prescription pain relievers. Some commonly prescribed opioid analgesic medications include oxycodone (OxyContin®), hydrocodone (Vicodin®), morphine, and methadone. These medications are prescribed to treat acute or chronic pain disorders ranging from moderate to severe.
Strong synthetic opioids like fentanyl are mostly used to treat extremely severe chronic pain, frequently in cancer patients.
As a fentanyl transdermal patch or intravenous formulation, it provides strong around-the-clock relief from advanced disease pain. However, illegally manufactured fentanyl has also increased in some areas due to its high risk of overdose and addiction. Another illegal opioid drug is heroin.
Risks of Opioids
Higher doses of prescription opioids pose greater risks. Doses over 100 morphine milligram equivalents (MME) per day have over two times the risk of misuse and overdose compared to lower doses. Even doses as low as 20-50 MME still present risks.
Long-term opioid use, even for a short period, such as a few days, can lead to physical dependence and addiction in some individuals. According to studies, one in four primary care patients who receive long-term opioid prescriptions also suffer from an opioid use disorder.
There are more dangers associated with long-acting and extended-release opioid formulations than with immediate-release ones. Their effects last longer, increasing overdose risk compared to short-acting pills.
Certain health conditions or traits may increase sensitivity to opioid effects and overdose risk. Older adults age 65+, people with respiratory or wasting diseases, and those with impaired strength are more vulnerable. Younger adults aged 18-25 and individuals with mental health or substance use disorders also face higher risks of misuse and addiction.
Opioid addiction remains a considerable public health issue due to its addictive properties and risks. One treatment option, Suboxone, has gained widespread use but also controversy over dental side effects.
According to TorHoerman Law, Suboxone contains buprenorphine and is used to treat opioid use disorder. While offering a safer approach than other opioids, its sublingual film form has been linked to severe tooth decay. The acidic film is proven to weaken enamel over time.
As a result, multiple lawsuits, such as the Suboxone lawsuit, have been filed against the manufacturer, Indivior, alleging failure to warn consumers properly.
The company only added a dental warning to packaging in 2022 after pressure from the FDA regarding this issue. The legal cases aim to hold Indivior accountable for not disclosing these dental risks associated with long-term Suboxone use.
What Is Opioid Use Disorder?
Opioid use disorder (OUD) is the term for an opioid use pattern that is problematic and significantly impairs or distresses the user. Key symptoms include withdrawal symptoms when not taking the drug, as well as a compulsion to seek out opioids despite their harmful effects. Opioid dependence and addiction are also terms sometimes used to describe OUD.
The risk of developing OUD is higher among those who misuse opioids. Opioid misuse includes taking higher doses than prescribed, more frequent use than directed, taking opioids to experience their psychoactive effects, or using someone else’s prescription opioids. Misuse of prescription opioids is a leading factor in the rise of OUD.
The misuse of opioids has become a serious public health crisis in the United States. As opioid misuse has increased, more pregnant women are also misusing opioids. This can jeopardize the health of both mother and baby.
Babies exposed to opioids in utero may suffer from neonatal abstinence syndrome (NAS), experiencing withdrawal symptoms after birth. Since some people switch to cheaper or easier-to-get illicit opioids, the expected availability of prescription opioids has also contributed to an increase in heroin use.
The far-reaching impacts of the opioid epidemic highlight the importance of preventing OUD through safe prescribing practices and treatment for those suffering from this chronic disease.
In conclusion, while opioids play an important role in managing severe acute and chronic pain, their use also carries significant health risks. Extended opioid therapy can potentially lead to physical dependence, addiction, and even overdose – especially at higher doses or in certain vulnerable patient groups.
It is vital that healthcare providers carefully consider the benefits and risks of long-term opioid treatment for each individual case. Close monitoring of patients on opioids is also necessary to mitigate dangers and address potential issues like misuse early on.